Continuity of care has a big impact on health outcomes, but can the NHS bring back personalised appointments?
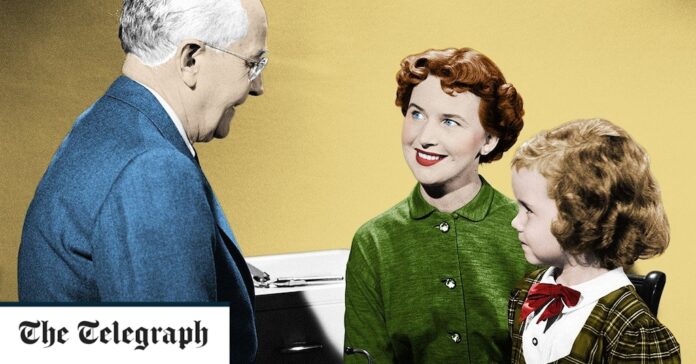
Remember the days when “going to the doctor’s” meant meeting the same, friendly face over the prescription pad? As children, one reassuring family GP held a cold stethoscope to our chests; in our adult lives, a “named” doctor confirmed our pregnancies, vaccinated our babies, perhaps even saw us through a cancer scare. When we walked into that consultation room, our GP recognised us and had a vague understanding of our medical history without having to start from scratch on a computer screen.
Much has been written about the seemingly-overnight move to remote or telephone consultation. Forty-nine per cent of appointments are now over the phone, compared with a mere 10 per cent in 2020. But even when you are lucky enough to get through to your practice these days, personalised appointments now seem as vintage as the tatty old magazine in the waiting room.
Finally, it seems the establishment is taking notice. Recently, the House of Commons Health Committee lamented the death of “cradle-to-grave” care, and called for the return of the “personal list”.
“The important relationship between a GP and their patients is in decline,” said committee member Rachael Maskell, MP for York Central. “Seeing your GP should not be as random as booking an Uber with a driver you’re unlikely to see again.”